Interoperability was established as a key facet of the World Health Assembly’s resolution WHA71.7, a global initiative to improve healthcare delivery by adopting a person-centric approach to digital health solutions.
And as more regulations around patient access, data use transparency, and security emerge, it’s clear that healthcare interoperability can’t be ignored
Committing to Standardization Protocols Will Allow for Improved Adoption at the Organizational Level
The role of standardization will be significant and will improve interoperability adoption throughout healthcare systems.
As there are complex overlapping rules and a diversity of healthcare data formats, like a structured electronic health record (EHR) versus an unstructured doctor’s note, standardization will only improve the data exchange process at its core.
According to HIMMS, there are four levels of healthcare interoperability to consider:
- Organizational interoperability
- Semantic interoperability
- Syntactic interoperability
- Technical interoperability
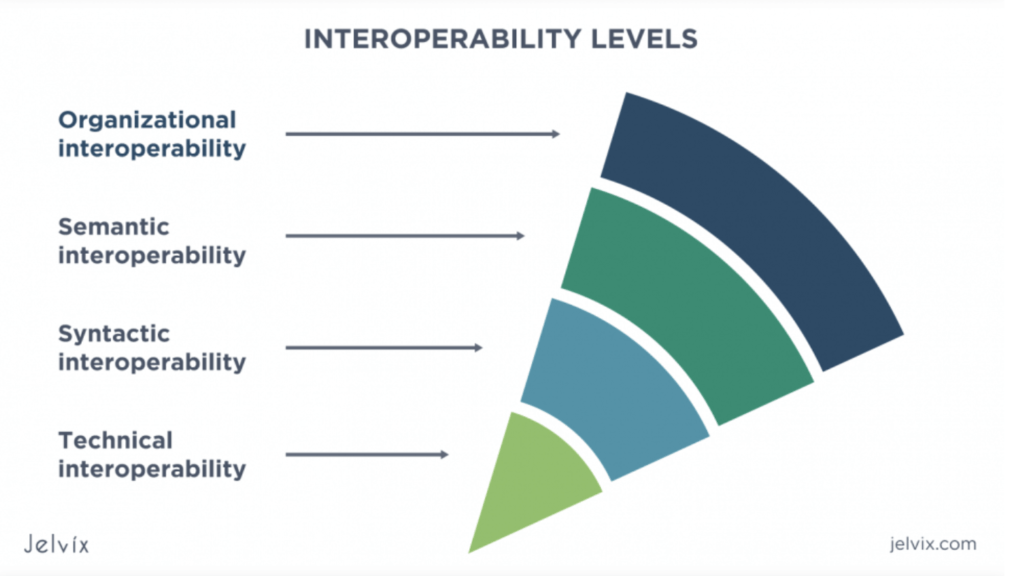
Each level of interoperability will require a different set of interoperability standards. These can broken down as follows:
- Vocabulary standards for technical interoperability
- Transport standards for structural interoperability
- Content standards for achieving semantic interoperability
- Adopt universal standards for organizational interoperability
An additional level of standards will also include identifier standards for patient privacy laws.
Innovative Tech Will Be Foundational to Technical Interoperability Success
Healthcare interoperability starts at the foundational level or technical interoperability. This is the most basic principle of true interoperability, in that one system or application communicates securely via data with another.
Ensuring that your systems can talk and accurately send and receive the necessary data securely is the first step, also known as the field level.
A great use case for achieving technical interoperability in cardiology clinics is GEMMS ONE, which applies common vocabulary or terminology standards, or common codes and terminologies to health and clinical concepts, to ensure that both sending and receiving machines will be able to interpret medical concepts with minimal ambiguity.
Among the most popular vocabulary standards are SNOMED-CT (intended for clinical terms), LOINC (intended for laboratory and clinical tests), CPT (intended for billing procedures), and ICD-10 (intended for diseases and injuries).
To achieve a basic technology level of interoperability, healthcare companies must adopt standardized coding that not only achieves communication standards but also encryption standards. Healthcare IT is one of the most susceptible industries to data breaches; therefore, healthcare interoperability must address the serious cybersecurity threats that will only increase.
Establishing robust encryption methods, separating access rights using the least privilege principle, implementing electronic document signatures, and applying a defensive-in-depth strategy can help resolve security issues and protect patient information. Regular updates of security protocols can ensure compliance with HIPAA and other regulations to fortify interoperable systems against cyber security threats.
Ensuring Efficient Transport Standards Will Improve Structural Interoperability
The ability of a receiving physician, clinical laboratory technician, pharmacist, or patient to interpret data received at the field level, also known as structural interoperability, involves the secure transfer process of data.
This requires that both of the communicating systems adopt a universal syntax, organization, and format standard during the healthcare data exchange.
Strict transport standards ensure that the data follows the specifications for data format, architecture, templates, and user interfaces of electronic messages so the data is received properly, the information is accurate, and the patient can be cared for in a timely manner.
Transport standards enable interoperability by using push and pull approaches to health data exchange. The common examples include DICOM (intended for transmitting medical images), Direct Standard (intended to carry C-CDA formatted data), and Fast Healthcare Interoperability Resource (FHIR, which uses RESTful APIs to share documents in XML, JSON, or RDF formats).
Adhering to these standards also addresses the poor data quality issue where disjointed or outdated health IT platforms send data containing low-quality information, such as irrelevant data, data missing crucial elements, and invalid information, all of which can compromise the accuracy of patient medical records and take away from the patient experience and lead to poor patient care.
Apply Content Standards for Semantic Interoperability
Achieving technical and structural interoperability allows for semantic interoperability, which is the ability for healthcare information to be fully interpreted and utilized by authorized parties in the exchange. Here you’ll want to apply communication standards to ensure the clinical and operational means of exchanging information remain unaltered and preserved at the field level.
Content interoperability standards provide a unifying structure and location for content shared in documents. They also indicate common sets of data that should be used in specific types of messages.
Consolidated CDA (C-CDA) and HL7’s newest version (V2) are the most common content standards as they allow for a streamlined approach between inter-provider and provider-patient communication. This is the semantic interoperability necessary for exchanging documents.
Content standards for the electronic data exchange at the semantic level improve the quality and safety of healthcare delivery. Beyond this, you’ll be making your data more accessible and understandable to patients, which means also considering how that data is interpreted by the user.
Developing user-friendly interfaces for patients is key. Patient portals should follow World Wide Web Consortium’s (W3C) Web Content Accessibility Guidelines and can improve patient access and empower patients to manage access to their electronic health information.
These considerations must be made throughout the innovation of artificial intelligence, generative AI and other workflow automation tools in healthcare. These will quickly become integrated into EHR systems and useful for interoperability and improving patient care.
The pivotal role of cloud platforms in securely receiving, transforming, and storing healthcare data is also a necessary consideration this year
Consider as well a consent management system to help ensure compliance with privacy regulations and allow patients to set preferences, giving them control over how their data is shared and utilized.
Address Global Privacy Concerns With Identifier Standards
Privacy and security standards are central to healthcare IT and address the issues of patient data safety and security. They are currently upheld by two main laws.
- In the USA healthcare system, the Health Insurance Portability and Accountability Act (HIPAA) sets standards that protect health information privacy.
- In EU healthcare systems, the General Data Protection Regulation (GDPR) establishes the privacy and security regulations related to information storage and processing in all areas, including healthcare.
They are aimed at defining who, when, and with what purpose providers can collect, access, process, and disclose patient health data.
Identifier Standards are universal methods of identifying healthcare providers and patients through the health system, such as Enterprise Master Patient Index (EMPI), Medical Record Number (MRN, for historical patient data for a hospital stay), National Council of State Boards of Nursing Nurse Licensing or NCSBN ID, and National Provider ID (NPI) for healthcare provider verification.
Choosing GEMMS ONE For Organizational Interoperability
Healthcare leaders know that achieving ongoing and reliable organizational interoperability will take a lot of work.
Adopt a reliable, common overarching standard, such as HL7 and FHIR mentioned earlier, as this will quickly become a relied-upon language for healthcare data exchange.
Protocols like FHIR are also gaining traction within the healthcare industry. FHIR offers a flexible and adaptable standard for the electronic exchange of healthcare data, providing a unifying language for disparate systems. Similarly, open APIs enable different healthcare applications to communicate and share data, promoting interoperability across a range of systems.
These protocols will help you achieve organizational interoperability, which covers legal, policy, social, and management components. Achieving this depends on the workflows and processes of each organization.
The use case for an EHR vendor like GEMMS ONE in improving organizational interoperability is significant, as GEMMS ONE provides EHR interoperability for different levels of responsibilities, systems integrations, and compliance through a patient-centric care approach.
Keeping patient-centric care in the strategic development of your healthcare’s interoperability system is very important. Without this focus, you might miss care coordination and easy wins.
A patient-centric focus does the following:
- Provide easy digital access to services and providers
- Use advanced analytics to provide personalized care and empower patients in their own healthcare decisions
- Better access to health records for informed patient choices
- Encouraging home-based care to improve accessibility and patient experience while allowing for proper care, which also includes feasible remote patient monitoring features and remote diagnostic capabilities
- Providing value-based care, or the prioritization of quality outcomes, early intervention, and preventive care
- Listening to patient feedback for the co-creation of healthcare services and policies
- Recognizing diverse needs and inclusivity for improved health outcomes.
While gaining interoperability at the organizational level is key for the seamless and secure enactment of data exchange between healthcare professionals and clinicians, it requires efficiencies in all of the other working components.
Patient-Centric Care Redefined
Clinicians agree that the lack of real-time access to clinical data as well as significant hurdles in interoperability can pose serious health threats.
Interoperability guarantees a high level of data accuracy by eliminating human factors and limiting the risks of mistakes. Unfortunately, while this need for improved operational efficiency is high in patient care, achieving a good level of interoperability in every organization requires a comprehensive approach and will take time not only due to the complex nature of it but also the added intricacies of the U.S. healthcare system.
Better interoperability contributes to improved patient outcomes, increased patient engagement, mitigated clinician burnout, reduced costs, fewer errors, and more accurate public health data for improved patient access to data (a core requirement of MIPPS).
The use case for software like GEMMS ONE in improving interoperability is significant, as this EHR system takes into consideration the demands for interoperability with different levels of responsibilities, systems integrations, and compliance.
Contact GEMMS ONE today to schedule a demo and see how we can improve interoperability in your cardiology practice.