Efficient data management and interoperability are crucial for navigating regulatory requirements and optimizing performance in healthcare programs like MIPS (Merit-based Incentive Payment System), especially given the industry’s constant changes.
With the recent changes to MIPS reporting requirements, healthcare providers seek innovative solutions to streamline their reporting processes while maximizing incentives and improving patient care.
Below, we will explore the 2024 changes to MIPS and how interoperability features in EHR software can revolutionize how cardiology providers approach MIPS reporting changes.
What is MIPS?
Established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the MIPS Program is pivotal in determining Medicare payment adjustments for healthcare practices.
By assessing a composite performance score, eligible clinicians stand to receive payment bonuses and penalties or remain unaffected by adjustments.
Launched on January 1, 2017, MIPS sets out to revolutionize the healthcare landscape, transitioning it from a fee-for-service model to one that prioritizes value-based care. Additionally, MIPS aims to ease the administrative burden on eligible clinicians while instilling confidence in the consistency of their annual payment updates.
At the heart of the Quality Payment Program (QPP), MIPS encompasses two core components: the Merit-Based Incentive Payment System (MIPS) and Alternative Payment Models (APMs). By consolidating previous Medicare initiatives, including the Physician Quality Reporting System (PQRS), the Value-Based Payment Modifier Program (VM), and the Medicare Electronic Health Record Incentive Program (EHR), MIPS streamlines reporting and incentivizes quality care delivery.
In addition to this, the Medicaid EHR Incentive Program aims to encourage healthcare providers to adopt and effectively use certified Health IT to improve patient care information exchange.
This initiative complements MIPS MVP and the Medicare Promoting Interoperability Program, ensuring alignment with Medicare Advantage and Medicaid services to enhance healthcare delivery.
Understanding MIPS Changes for 2024
One of the significant updates in the final 2024 rule is the decision to maintain the penalty threshold at 75 rather than increase it to 82, as initially anticipated.
This decision will likely relieve many eligible clinicians (ECs) affected by MIPS, including cardiologists who rely on accurate reporting for optimal reimbursement.
Additionally, the 2024 final rule retains the methodology for measuring scores and achieving points with no notable alterations. This consistency provides a stable framework for cardiologists to navigate MIPS reporting requirements.
2024 Quality Modifications
For quality category adjustments, the electronic case reporting period remains at 12 months, and six quality measures, including one high-priority measure, persist for 2024. This stability ensures that cardiologists can continue focusing on delivering high-quality care while meeting MIPS reporting obligations, including those related to prior authorization.
Notably, the 2024 final rule raises the data completeness threshold from 70% to 75%. Cardiologists must report at least 75% of all eligible instances for the reporting year to ensure compliance and maximize points for each quality measure, including those related to prior authorization.
A proposed rule change for future years, specifically 2026 and 2027, suggests modifying this threshold to 80%, which cardiologists should consider for future planning.
There are 198 quality measures available for the 2024 Quality Measure changes, including those pertaining to prior authorization. Of these, 13 new quality measures have been introduced, 11 have been removed, and 59 have undergone modifications.
This evolution underscores the importance of staying informed about updates relevant to cardiology practice, including changes in prior authorization requirements.
How Gemms One Interoperability Can Streamline the MIPS Reporting Changes for Cardiology Practices
Efficient data management and interoperability are crucial for navigating regulatory requirements and optimizing performance in healthcare programs like MIPS, especially in specialized fields like cardiology.
Near constant changes within the healthcare industry, make innovative solutions like Gemms One Interoperability essential for cardiologists aiming to streamline their reporting processes while maximizing incentives and improving patient care.
Below, we will explore how Gemms One Interoperability can revolutionize the way cardiologists approach MIPS reporting changes.
Improved Provider Access
Provider access refers to the ability of healthcare providers, such as physicians, nurses, and other medical professionals, to access relevant patient information, medical records, and clinical data within healthcare systems. It encompasses the permissions, tools, and technology infrastructure required for providers to retrieve, review, and update patient records efficiently and securely.
Effective provider access ensures that healthcare providers have timely access to accurate and comprehensive patient information, enabling them to make informed clinical decisions, coordinate care effectively, and deliver high-quality medical services. Provider access often involves electronic health record (EHR) systems, patient portals, and other health information technologies that facilitate seamless communication and data exchange between healthcare providers, patients, and other stakeholders.
In essence, provider access plays a crucial role in optimizing healthcare delivery by empowering providers with the information they need to deliver timely, coordinated, and patient-centered care.
Seamless Data Integration
Gemms One Interoperability offers seamless integration with Electronic Health Record systems, practice management software, and other data sources tailored to cardiologists’ needs.
This integration enables the healthcare provider to effortlessly aggregate and analyze data from multiple sources, ensuring comprehensive reporting across all MIPS performance categories specific to cardiology practice.
The Electronic Health Record Incentive Program, also known as Meaningful Use, was established to encourage healthcare providers to adopt and effectively use certified EHR technology to improve patient care.
Eligible professionals and hospitals could qualify for financial incentives by demonstrating meaningful use of EHRs in ways that positively impact patient outcomes, safety, and health information exchange.
The program initially aimed to enhance healthcare quality, efficiency, and coordination through the adoption of electronic health records across the healthcare system.
However, it has since evolved, with the focus shifting from incentives for adoption to promoting interoperability, data exchange, and patient engagement through programs like the Promoting Interoperability category within MIPS.
Advanced Analytics
The platform’s advanced analytics capabilities empower cardiologists to gain valuable insights into their performance metrics, identify areas for improvement, and track progress toward MIPS reporting goals.
By leveraging specialized analytics for cardiology, Gemms One Interoperability provides actionable data-driven insights to optimize performance and maximize incentives, from quality measures to cost containment strategies relevant to cardiologists.
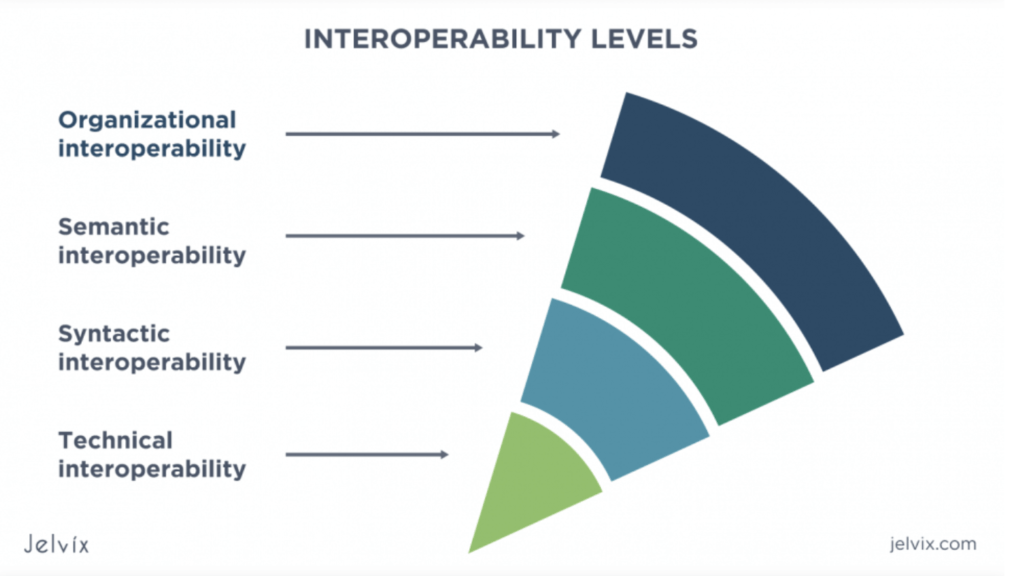
Interoperability Standards Compliance
Gemms One Interoperability adheres to industry standards and regulations, ensuring seamless data exchange and interoperability specific to cardiology practice.
By leveraging standardized data formats and protocols relevant to cardiology, healthcare organizations can enhance information exchange efficiency and quickly meet MIPS reporting requirements, ensuring compliance while focusing on delivering high-quality care.
Patient Engagement Tools
Engaging patients in their care is paramount for achieving success in MIPS reporting, especially within the Promoting Interoperability category, where patient access and engagement are key metrics. Gemms One Interoperability recognizes this importance and offers tailored patient engagement tools designed to meet cardiology practice’s unique needs.
These tools empower cardiologists to communicate effectively with patients, providing them with personalized care plans and fostering active participation in their treatment journey.
By facilitating health information exchange specific to cardiology, Gemms One Interoperability ultimately enhances patient outcomes and satisfaction, ensuring that patients receive optimal care tailored to their individual needs and preferences.
Customizable Reporting Dashboards
Gemms One Interoperability features customizable reporting dashboards designed to visualize key performance indicators relevant to cardiology practice.
Cardiologists can monitor MIPS reporting progress in real-time, track quality measures specific to cardiology, assess improvement activities, and analyze cost containment efforts, leveraging intuitive dashboards tailored to the unique needs of cardiology practice.
Leveraging GEMMS Interoperability for Streamlining Medical Billing and MIPS
As cardiologists navigate the evolving landscape of MIPS reporting changes, embracing innovative solutions like Gemms One Interoperability can significantly streamline reporting processes, enhance data management capabilities, and drive better patient outcomes.
By leveraging advanced technology, seamless data integration, and actionable insights specific to cardiology practice, healthcare organizations can adapt to regulatory requirements, maximize incentives, and ultimately improve the quality and efficiency of care delivery in cardiology.
With Gemms One Interoperability, the future of MIPS reporting for cardiologists is brighter than ever, empowering providers to thrive in an increasingly complex healthcare environment.
Feel free to reach out to us to learn more about how Gemms One Interoperability can streamline MIPS reporting for your cardiology practice and enhance patient care. Our dedicated team is available to provide personalized demonstrations, answer any questions you may have, and guide you through the process of implementing our innovative solution.
Contact us today to schedule a demo to take the first step towards optimizing your MIPS reporting and improving outcomes for your patients.